By: Stephen Jarrell LCSW, LCAC, ACSW, Executive Director, Headwaters Counseling and Vanessa Jones, MS, LMHC, Associate Director, Headwaters Counseling
Although the mind and body are often viewed as operating separately, mental and physical health are actually very closely related. Good mental health can positively affect physical health. Certainly the opposite is also true where poor physical health can in turn impact mental health.
Mental health services for adults have become much more widely accepted in the last few years, especially during the COVID-19 pandemic. Mental health services have become less stigmatized, mysterious, and are discussed much more openly. Those willing to discuss mental health issues often speak with courage and compassion which opens the doors to overall better mental health for all.
The same is not necessarily true for children. We expect children to be naturally resilient, and cooperative. The National Institute for Mental Health says that, even in ideal environments, raising a child can be challenging. “Even under the best circumstances, their behaviors and emotions can change frequently and rapidly. All children are sad, anxious, irritable, or aggressive at times, or they occasionally find it challenging to sit still, pay attention, or interact with others. In most cases, these are just typical developmental phases. However, such behaviors may indicate a more serious problem in some children.”
Many mental disorders can begin in childhood including anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder, depression and other mood disorders, eating disorders, and post-traumatic stress disorder (PTSD). Without treatment, these mental health conditions can prevent children from reaching their full potential. Many adults who seek mental health treatment reflect on the impact of mental disorders on their childhood and wish they had received help sooner.
Staying mentally well should be given the same priority as keeping physically fit for adults and children. We will all need medical services at some point in our lives, and the same may be true of mental health services. Factors such as lifestyle, life events, and genetics may determine the need, type, and frequency of these services and we should all strive to keep ourselves mentally and physically well. Seeking treatment earlier, rather than later, is a good preventive measure regardless of age.
Good mental health in a child
So what does good mental health look like in a child? Good mental health in a child allows children to think clearly, develop socially, and learn new skills. Being mentally healthy during childhood means reaching developmental and emotional milestones, learning healthy social skills, and how to cope when there are problems. Mentally healthy children have a positive quality of life and can function well at home, in school, and in their communities. Additionally, good friends and encouraging words from adults are all important for helping children develop self-confidence, high self-esteem, and a healthy emotional outlook on life.
We may not recognize our own poor mental health
What is poor mental health? Simply put, this is when our mental health is not what we want it to be. Finding it difficult to manage how we think, feel, and act with respect to daily stresses could be a sign of poor mental health. Having continuous episodes of poor mental health could indicate a problem.
We, as adults, are not the most astute at determining if we have mental or physical health issues that need to be addressed. Often it is someone close to us who will notice that we may be struggling before we notice it ourselves. This is the same for our children. We know when something may be wrong with a child—but may not know what to attribute it to, or even find words to articulate the problem. A child might be a tad more irritable, sad, frustrated, sleeping too much or even too little. While these behaviors don’t necessarily indicate a mental health need or issue, behavioral changes are usually fairly good benchmarks to identify when something may be amiss.
It’s important to keep communication open and to be honest and empathetic when inquiring about a change in behavior. Come from a place of compassion and concern. If the behaviors are negatively impacting other parts of a child’s life, or even a family’s life, then there is a reason to be concerned. One may not typically seek medical attention for a simple cold, but if the symptoms get worse or hang around longer than expected, we seek treatment. The same is true of mental health issues—if symptoms and feelings hang on or negatively impact our lives, we should seek professional assistance.
The pandemic’s impact on everyone’s mental health
During the COVID-19 pandemic, concerns about mental health and substance use have grown, including concerns about suicidal ideation. In January 2021, 41% of adults reported symptoms of anxiety and/or depressive disorder—a common trend that has been identified since the spring of 2020. Representative panel surveys were conducted by the Centers for Disease Control and Prevention (CDC) among adults aged ≥18 years across the United States during June 2020. 13% of adults reported new or increased substance use due to coronavirus-related stress, and 11% of adults reported thoughts of suicide in the past 30 days. Suicide rates have long been on the rise and may worsen due to the pandemic. Early 2020 data shows that drug overdose deaths were particularly pronounced from March to May 2020, coinciding with the start of pandemic-related lockdowns. And, Indiana has been particularly hard hit with suicide rates and overdose deaths.
None of this is new information regarding adults; however, very little data is available about children. The available statistics for adolescents was collected pre-COVID-19. According to data from the National Survey on Drug Use and Health, an estimated 13% of U.S. adolescents aged 12-17 experienced at least 1 episode of major depressive disorder in 2017, yet 60% of these individuals did not receive treatment for their illness.
In addition, survey results from the CDC demonstrated increasing rates of US high school students experiencing persistent sadness or hopelessness (from approximately 26% in 2009 to 37% in 2019), serious contemplation of suicide (from 14% to 19%), suicide planning (from 11% to 16%), and incomplete suicide (from 6% to 9%).
Helping children cope with the return to school
Generally speaking, children do not have the same ability to cope as adults and they do not have the power to make decisions as adults do.
Going or returning to school this fall for both children and adults has been a continued test of patience. Regardless of political positions, there has been a great deal of turmoil surrounding vaccinations, masks, social distancing, school rules, and a huge societal division that seems to be at a stalemate. As adults, most of us feel we have been through the wringer—we’re tired, frustrated, hoping for things to be safe, and getting back to whatever normal looks like. Our children are no different but they are watching, learning, and looking to the adults in their lives for answers and reassurance. And, perhaps, they find that reassurance lacking.
Returning to school provides a perfect opportunity for parents to observe closely, pay attention, and identify changes in behavior, attitudes, eating patterns, and sleep habits of their children. Early identification of issues, accurate diagnosis by a professional, and effective treatment of mental health and substance abuse in school-aged children can alleviate enormous suffering and heartbreak for the future. If in doubt, ask questions, and seek verification from school personnel and administrators. Check your observations against theirs and trust your instincts when it comes to your child.
Don’t hesitate to seek assistance
If you or your child is in need of a mental health checkup, a conversation, or a family or group discussion, reach out for professional help.
There are many resources for parents and caregivers who want to know more about children's mental health. Learn more about:
- Recognizing mental health problems in children, how they are affected, and what you can do
- Diagnosing and treating children with mental health problems
- Talking to children and youth after a disaster or traumatic event
Get immediate help for your child. Learn more here.
Seek immediate assistance if you think your child is in danger of harming themselves or others. You can call a crisis line or the National Suicide Prevention Line at 1-800-273-TALK (8255).
For an appointment with a licensed Headwaters therapist, call: 260-744-4326, or email: Alicia.staneck@headwaterscounseling.org.
- Office location: 2712 South Calhoun Street, Fort Wayne, IN 46807
- Office hours: Monday through Thursday, 8 a.m.-8 p.m.; Friday, 8 a.m.-12 p.m.
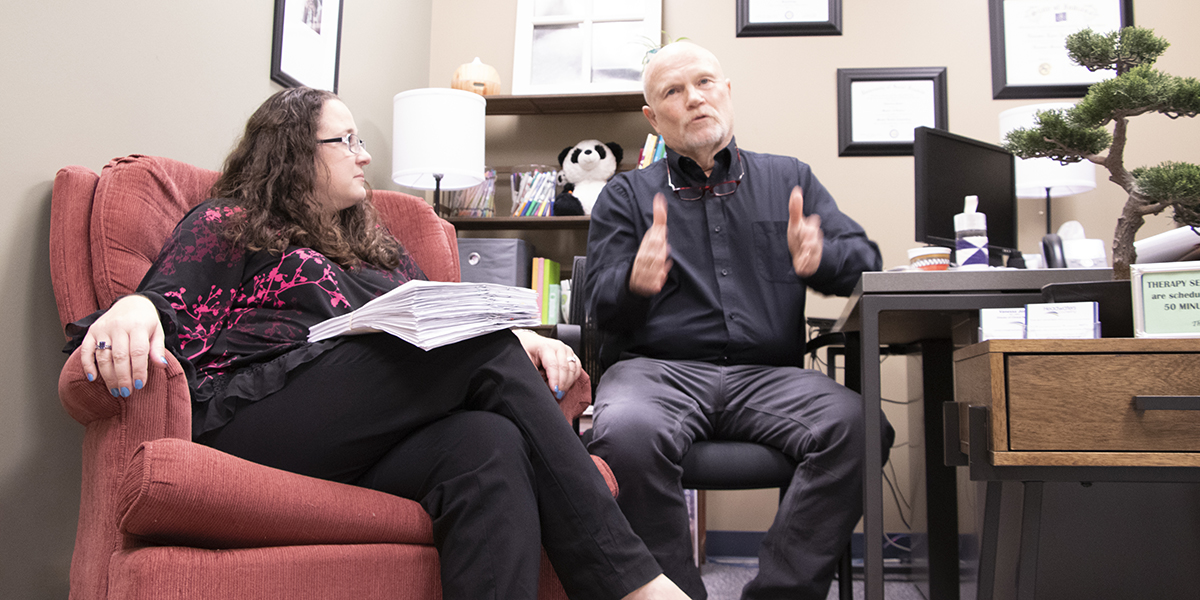 Pictured above: Vanessa Jones, MS, LMHC, Associate Director, Headwaters Counseling and Stephen Jarrell LCSW, LCAC, ACSW, Executive Director, Headwaters Counseling
Pictured above: Vanessa Jones, MS, LMHC, Associate Director, Headwaters Counseling and Stephen Jarrell LCSW, LCAC, ACSW, Executive Director, Headwaters Counseling
About Headwaters Counseling
Headwaters Counseling has been providing trusted mental health counseling, outreach, and services for those in need for more than 50 years. Headwaters counseling promotes, develops, and empowers individuals, families, and communities to have healthy relationships and make positive life choices so people and families can live meaningful lives.
As a private, not for profit, 501(c)(3) agency in Fort Wayne, Indiana, Headwaters Counseling provides outpatient counseling services for people with behavioral health needs or at risk of harmful involvement with alcohol or other drugs.
A member of the Alliance for Children & Families and the Indiana Family Service Council.